In the first three parts of this pain relief series
Your Pain Relief Plan Introduction
I discussed why we feel pain and how the degree of pain felt due to lifestyle factors could vary widely from one individual to the next. Also, when long term, typically over 3 months, the brain would effectively lock the pain in. Emotional trauma, even as far back as childhood, had been found to lock in pain for almost a lifetime.
I then went into more detail about how pain works and discussed the implications of ageing and the differences between acute and chronic conditions, and the most effective ways of treating these.
With this as a background, we will now explore the causes of nerve-related neuropathic pain and how it gets locked into the body. This in turn clarifies why exercise and /or some drugs may not be the correct pain relief solution when suffering neuropathic pain.
Pain Assessment
It should be clear by now that it is vital to be properly assessed by a qualified therapist before treatment starts. Otherwise totally, the wrong treatment could be provided. But we need to go back one stage further to obtain an effective assessment.
In a separate series of blogs on A Different Perspective on Your Physiotherapy Assessment, I explained the vital steps needed for a successful assessment before even starting the physical assessment. This included creating the right environment to build connection and trust, without which a detailed understanding of the back story behind the problem could not be effectively communicated.
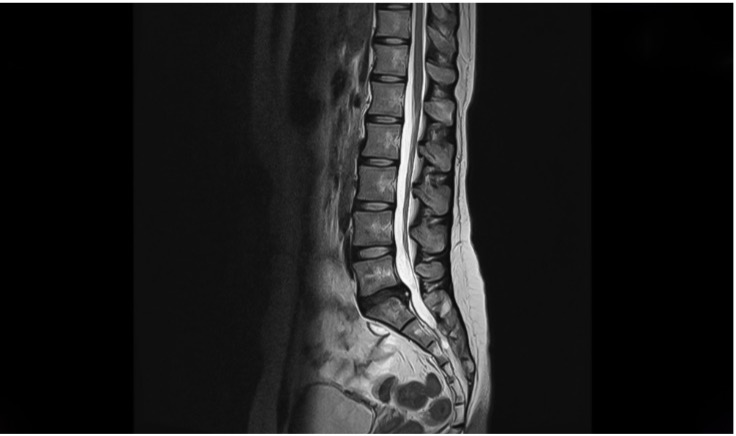 Even with this approach, therapists, however qualified, are trained to manually assess conditions but ultimately can only come up with a provisional diagnosis. To confirm this diagnosis, additional scans, such as EMG to look at nerve function, MRI, Xray and ultrasound may be needed. Even then, some conditions are invisible to such scans. Scans may thus be able to eliminate some causes, but not able to confirm the actual cause. A good example is that neither MRI nor X-ray can see muscle spasms, the latter being responsible for a lot of neuropathic problems, such as sciatica.
Even with this approach, therapists, however qualified, are trained to manually assess conditions but ultimately can only come up with a provisional diagnosis. To confirm this diagnosis, additional scans, such as EMG to look at nerve function, MRI, Xray and ultrasound may be needed. Even then, some conditions are invisible to such scans. Scans may thus be able to eliminate some causes, but not able to confirm the actual cause. A good example is that neither MRI nor X-ray can see muscle spasms, the latter being responsible for a lot of neuropathic problems, such as sciatica.
Holistic Treatment
Those of you who have previously had a dislike or mistrust of the term holistic, should by now, if you have read my previous three parts of this series, realise that even latest scientific technology has measured non scientific factors as having significance. It has been confirmed that pain is modulated by factors such as attention, anticipation, empathy, placebo, meditation, fear, anxiety, posture, emotion and movement. This, in turn, has confirmed the benefits of a more holistic approach to assessment and treatment.
Our ancient Doctors, called Shamans at the time, always knew that the link between mind and body was key to healing. Those same ancient Doctors would look at the whole body, the mindset, fitness, diet and lifestyle of the patient. They also knew that the level of social support the patient had was a key factor.
Latest research is confirming these same links between mind and body as it has now been found that without consideration of the whole, Long-COVID sufferers, for example, will struggle to heal.
Further, we know that the backstory and meaning to the patients’ pain is
essential to understanding the suffering. Without listening to and understanding the backstoryand
 meaning, the minds’ healing process cannot start. Evidence suggests that in chronic and complex pain cases, there are likely to also be problems with fear, mood and personality.
meaning, the minds’ healing process cannot start. Evidence suggests that in chronic and complex pain cases, there are likely to also be problems with fear, mood and personality.
The negative factors in our modern day lifestyle, particularly as the world is experiencing a pandemic, are worsening. As a consequence, it is feared that that there will be both an increase in the rate of chronic pain cases and the severity of its impact will have widespread social implications.
The case for a more holistic approach is thus building if we want to successfully fight this growing threat.
Pain Relief – The Way Forward
Pain, as we have seen, can result from a multitude of causes. Pain can be acute or chronic, physical or emotional, physical or neuropathic and is impacted by other factors including emotion, mindset, exercise, nutrition and lifestyle.
Clearly, the therapist you choose needs to be properly qualified to assess and treat you both physically and holistically and incorporate the significance of your mindset, fitness, diet, lifestyle, emotional support network and be empathetic to your story.
In the final part of this blog series Pain Relief – Your Escape Plan I will explain in more detail the approaches to treating the symptoms of chronic pain problems and highlight the differences between maintenance and wellness. Lastly, I introduce our clinic's own 4 Keys To Health approach and how it fits with Wellness.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
In parts 1 and 2 of this pain relief series:
Your Pain Relief Plan Introduction
I discussed why we feel pain and how the degree of pain felt due to lifestyle factors could vary widely from one individual to the next. Also, when long term, typically over 3 months, the brain would effectively lock the pain in. Emotional trauma, even as far back as childhood, had been found to lock in pain for almost a lifetime.
I then went into more detail about how pain works and discussed the implications of ageing and the differences between acute and chronic conditions, and the most effective ways of treating these.
With this as a background, we will now explore the causes of nerve-related neuropathic pain and how it gets locked into the body. This in turn clarifies why exercise and /or some drugs may not be the correct pain relief solution when suffering neuropathic pain.
 We have explained that the pain signal is passed through the nervous system up to the brain. As an analogy of a nerve cord, imagine a tight bundle of tiny electrical wires and that each one of these wires is connected to a specific part of the body. Imagine, as an example, an injury and inflammation to your foot and that one such ‘wire’ is connected to a very small part of that injured area. It will send a pain signal to the brain, and of course, the brain knows exactly where the wire is connected in the body. The result is you will feel pain in your foot.
We have explained that the pain signal is passed through the nervous system up to the brain. As an analogy of a nerve cord, imagine a tight bundle of tiny electrical wires and that each one of these wires is connected to a specific part of the body. Imagine, as an example, an injury and inflammation to your foot and that one such ‘wire’ is connected to a very small part of that injured area. It will send a pain signal to the brain, and of course, the brain knows exactly where the wire is connected in the body. The result is you will feel pain in your foot.
Now let’s go one stage further. That nerve bundle travels down your spine until it reaches the point at which it exits the spinal cord and passes down your leg to your foot. Imagine I could find that exact same wire in your spine. If I were to squeeze it, your brain would interpret that as a pain signal linked to your foot. You would feel exactly the same foot pain, but the problem this time is in your back. You may or may not have a real problem in your foot, but you would still feel pain in your foot.
Long-term pressure on a nerve will cause it to become super-sensitive and send pain signals even when there is no injury
Now, let’s go another stage further again. Imagine that nerve in your spine had previously been strangled for a period of time by a tight muscle contracture. Extended pressure on a nerve will cause it to function incorrectly and it will become ‘super-sensitive ’. That nerve will now send pain signals to the brain even when there is no current injury. In effect, the previous injury is locked in. Imagine a faulty wire having a similar effect.
’. That nerve will now send pain signals to the brain even when there is no current injury. In effect, the previous injury is locked in. Imagine a faulty wire having a similar effect.
Pain like this is called neuropathic pain because the nerve is super-sensitive.
The Do’s and Don’ts of Exercise
It’s not necessarily the case that exercises are appropriate at the start of treatment, as in some cases exercises, incorrectly timed, will make matters worse, not better. Neuropathic pain resulting from a trapped nerve is an example where exercises should not be given until the trap has been removed, allowing the nerve to move freely.
As an analogy, imagine I grabbed your wrist so hard that it hurt. Your reaction might be to try to pull your arm and wrist out of my grip. But if my grip is too strong, all that will happen is that your arm will ache and your wrist will be very sore. Yanking on a trapped nerve by exercising will have the same result. Exercise prescription needs to wait until the nerve is no longer trapped.
The Pro’s and Cons of Pain Medication
Pain may be a signal that something is wrong, but at best it’s not pleasant and at worst it can prevent normal daily living. If long term, it can cause depression and a loss of will to live. Thus, medication is an important part of our arsenal to control the pain until the cause of the pain has been established and then successfully treated.
There are, however, downsides to medication. The first and most obvious is that the medication works by masking or blocking the pain signals and does not treat the actual cause of the pain. Further, by masking the pain, it prevents us from getting the warning that something is wrong. Thus, we may continue to do the very things that the pain is trying to warn us not to do. If used long term, medication may, as a consequence, exacerbate the problem.
Opioids are ineffective in treating chronic pain
Secondly, when the pain level is severe, opioid based drugs are often prescribed, with no differentiation between acute and chronic conditions. The problem here is that chronic conditions will most likely need long term medication and opioids are naturally addictive. In fact, so much so, that opioids have caused the majority of drug addictions in the USA. To make matters worse, opioids have been recognised for some time as being ineffective in treating chronic conditions.
Thirdly, most drugs have negative side effects and long-term use can be dangerous.
To summarise, trapped nerves will cause neuropathic pain, a form of locked in pain which in itself can be misleading, as incorrect diagnosis could lead to treatment of where the pain is perceived, instead of where the cause of the problem resides.
It thus should come as no surprise that exercising, which will mean pulling on nerves to allow movement, will only make matters worse if those nerves are trapped.
Drugs are an effective short term solution, but care should be taken to avoid opiates when dealing with chronic conditions, as it is well proven that opiates are ineffective in such cases.
In the next part of this pain relief series Your Pain Relief Plan Part 4 I will discuss the assessment and the scientifically proven importance of holistic factors.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
In part 1 of this series, Your Pain Relief Plan Introduction I discussed why we feel pain and introduced the concepts that the degree of pain felt could vary widely from one individual to the next due to lifestyle factors. Also, when long term, typically over 3 months, the brain would lock the pain in. Emotional trauma, even as far back as childhood, has been found to lock in pain for almost a lifetime.
In part 2 of this pain relief series, I will get into more detail about how pain works and discuss the implications of aging and the differences between acute and chronic conditions and the most effective ways of treating these. But first, a quick look at the brain, how it has evolved and how this relates to processing pain.
Read on
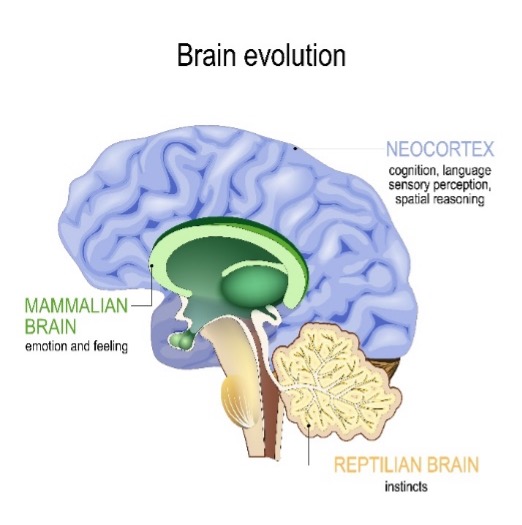
The oldest part of the brain is the reptilian brain, which deals with basic survival instincts. Next came the mammalian brain, which added the ability to feel emotion. The third part is the human brain, the Cortex, which gives us our human qualities of cognition, sensory perception and spatial reasoning and is in charge of the human decision making process.
Your nerves transmit pain signals. Inside your nerves you have sensors for temperature, stress, movement, pressure, immunity molecules and blood flow. Similar to car sensors, any damage or fault to any of these sensors will put a light on your dashboard, to alert you of a problem. The nerve does the same thing by increasing pain.
These pain impulses travel up the spinal cord, to a part of the brain which acts like a router (called the thalamus, which sits on top of the reptilian brain) and as a simple analogy, this router makes phone calls to other parts of the brain. Thus it acts like a hub on a wheel, sending out and gathering information from various parts of the brain. For example to:
- the sensory cortex (which interprets the sensory nature of the pain)
- the mammalian amygdala (which assesses the level of fear, as it is the emotional centre, and decides if the body needs to shut down digestion, cell division, circulation etc.)
- the neocortex (which is in charge of the human decision-making process).
Once information is gathered, the thalamus sends it forward, like a train leaving a station, through the limbic system ( the mammalian brain) where emotions are added on the train journey. Thus a person who is fearful or anxious will feel more pain. The train journey ends at the human brain where a decision of the level of pain felt is made. It is vital to understand that the degree of pain felt is not directly related to the initial cause of the pain signal, as there are many factors to consider, such as:
- Body sensation and location
- Movement – muscles may need to brace the area
- Focus & concentration
- Fear response
- Memory area recalling previous similar experience
- Motivation - processes pain
- Stress response - weight, digestion, sleep, temperature
All factors interact to decide on the suffering experienced. This may have little to do with the degree of injury and hence makes it clear that a qualified and knowledgeable therapist is needed to properly diagnose and treat the injury.
The Consequences Of Aging
As we age, we need to put more care into diet, supplementation, exercise, and our workload. It sounds simple, but many of us fail to even acknowledge that as we get older, we have to change the way we use our bodies. As we age, naturally occurring enzymes are fewer, inflammation is greater, and the production of inflexible scar tissue becomes much more extensive. Therefore, long-term solutions for pain relief also need to address our ongoing biochemical changes.
Sleep quality tends to deteriorate and ongoing deprivation can lead to symptoms virtually indistinguishable from widespread pain, fatigue and diffuse tenderness. Early evidence also shows that anxiety, depression and sleep disturbances have been common reactions to the COVID pandemic. Thus the problems faced by Long COVID sufferers are likely to be with us for many years to come.
What is the difference between Acute and Chronic Pain?
Acute pain is a safety mechanism located in the reptilian brain, the oldest part of the brain. It’s this ancient reflex system that makes you quickly take your hand out of the fire. Acute pain is typically pain which has resulted from a recent injury, such as a twisted ankle, bruised or torn muscle. In most cases acute pain needs immediate treatment and is usually resolved within a few treatment sessions combined with exercise prescription.
Chronic pain, by its nature, may not be resolvable
Chronic pain is long term pain, beyond 3 months, as the brain has hard wired the pain in by that time. Chronic pain can occur because of numerous conditions, such as emotional pain, joint wear and tear (osteoarthritis), spinal disc thinning, bulging or rupture, bone thinning (osteoporosis), unresolved tendon or ligament damage, to name but a few. Chronic pain, by its nature, may not be resolvable. It may need a lot more treatment than acute pain to bring down to acceptable levels and will benefit greatly from ongoing maintenance or wellness treatment to prevent reoccurrence.
Modern science confirms benefits of a more holistic approach
Latest neuro imaging technology, which can see the electrical activity in the brain in response to different lifestyles, has allowed the world to delve deeper into the understanding of chronic pain. It has confirmed that pain is modulated by factors such as attention, anticipation, empathy, placebo, meditation, fear, anxiety, posture, emotion and movement. This, in turn, has confirmed the benefits of a more holistic approach to assessment and treatment.
This new insight into chronic pain helps explain why, for example, X-rays showing the degree of osteoarthritis in joints has no correlation to the pain being felt.
To summarise, we have shown how each persons brain can process pain differently, to the extent that one person may feel tremendous pain, when another, with essentially the same condition, might feel little or no pain at all.
The availability of latest MRI scanning technology has verified that many non physical factors can impact the way pain is handled in the brain. This in turn supports the benefits of a more holistic approach to assessment and treatment.
Acute problems are usually caused by a recent injury and are best treated promptly, whereas chronic problems are longer term and tend to be related to the aging process. Chronic pain in many cases cannot be resolved and lends itself to a longer term control of symptoms, rather than treatment of root cause as with an acute injury.
In my next blog Your Pain Relief Plan Part 3 I will explain neuropathic pain and the effectiveness of both exercise and drugs and where these may be the wrong solution.
If you are in pain, then it’s important to get help as soon as possible. It is even more important if you have been in pain for an extended period, as you may be risk of your pain becoming locked in and the degree of pain you may feel may not be consistent with the severity of the cause.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
Great news. The sun is shining, and it’s holiday time!
Most of us have been couped up for the best part of a year, probably getting a lot less exercise than normal and possibly desperately needing some treatment for pain. Every year we get a surge of clients who have put their back out and need urgent help to resolve back pain before their holiday. This year it’s likely to be a bigger surge due to the relatively low activity due to COVID dragging on.
We are here to help and we will no doubt be able to get you out of pain in time for your holiday. But it’s important to realise that in most cases we won’t have enough time to completely fix the problem, so you will need to be a bit careful on your much looked forward to holiday.
Here is some simple advice to help you avoid ruining your holiday
First, let’s understand pain a little. When we are in pain, it’s difficult to get it off our minds. But once it’s gone, you can’t remember it, can you? You can remember you didn’t like the pain, but you can’t recreate the pain in your mind. There lies the risk.
Once the pain is gone, it’s forgotten and we feel good. Then we do stupid things and the pain comes back with a vengeance. What is one of the main culprits? Suitcases.

If you think about basic health & safety when picking things up, the rule is bend your legs, not your back. It makes sense, but not easy to do when putting a heavy suitcase in the boot of the car, or fighting to get the suitcase off the conveyor at the airport. Worse yet, one sure way of putting your back out is to lift and twist as the same time. What do you do when you take a suitcase out of the boot? You are in the way, so you twist and put the suitcase down! Ouch, home goal. Now for the Physiotherapy
Stop and think
Try two lighter suitcases instead of one heavy one. Bend your legs putting the suitcases in the boot, or even get two of you to do it. When you take a suitcase out of the boot, avoid twisting, instead rotate on your feet, like a robot.
Be extra careful with airport conveyors. They tend to be a free for all, and fighting to get a suitcase off before it goes past is a sure way to put excessive lifting and twisting loads on your back.
We have had many clients who ruined their holiday before it started. Don’t let that be you.
If you are in pain, we can help
Call 01889 881488 Now
Jean, Erica & Charlotte will be happy to help
So, how do you choose your physiotherapy clinic in seven easy steps?
-
Physiotherapy skills and qualifications
The most important question - is the physiotherapist appropriately qualified and is there any evidence of ongoing learning and development? Although principals remain consistent, the skills and style of approach can be different as can the aftercare. Please make sure you get reassurances of qualifications and can see ongoing development of therapists.
-
Clinic Location
If you need physiotherapy, it is important to consider a local physiotherapist or one that is convenient to you. At Nicky Snazell Clinic we do provide specialist physiotherapy to clients from all over the world who come to Nicky for healing, but in general, we would recommend that you consider a therapist who is within a commutable distance of your work or home location. A commutable distance is 40-60mins for the right care, Nicky Snazell Pain Relief Clinic service; Stafford, Lichfield, Cannock, Rugeley & Stone.
-
Style of approach
Like people, physiotherapists are all different. While we hope that they all subscribe to the highest possible standards and approaches, it is important that you make sure that from the initial consultation you feel connected with your therapist and their unique style of approach.
Consider the following:
- Have your questions been answered?
- Did you feel a connection with the therapist?
- Are you clear on the next steps?
- Did the therapist explain costs?
-
Getting to the root cause
Spending time to find the root cause of pain is more important than the treatment itself. We find some clients have pain that is the result of unresolved childhood issues, bereavement and work-stress for example. Without spending the time to really understand your unique situation, often it can be like treating the surface of the problem and not the long-term view of the issue.
-
Ongoing Physiotherapy care
Once your initial condition and pain are 'fixed', ongoing care is essential. As they say, prevention is better than cure, so periodic check-ups and follow-ups will help ensure that you are maintaining your health. We quite often treat sports injuries and also recommend massage for clients which can relax and rejuvenate you avoiding the aggravation of the problem area.
-
Other services
Sometimes you may receive physiotherapy which can show that you would benefit from other services such as electro-acupuncture, the aforementioned massage. Does your therapist offer other services to support your wellbeing?
-
Customer service
A good physiotherapy clinic has a team who can facilitate customer support and great customer service, like helping you to book your appointments, reminders and periodic communication in the form of useful insights, tips and observations to help.
If you are looking for a Physiotherapist why not give our team a call: 01889 881 488
This is the fifth part in a series of blogs looking at the process of a physiotherapy assessment and treatment plan. If you have missed the 4 earlier blogs, then here are the links:
A Different Perspective On Your Physiotherapy Assessment
The Subjective Physiotherapy Assessment
The Subjective Physiotherapy Assessment – Part 2
Your prescription is the final part of the physiotherapy assessment process. After we've got a connection. We have learned who your authentic self is. We’ve gone through the four keys analysis, to assess your immune system and general health. We have worked out what’s going on with you in terms of food, movement, stress, lifestyle and the way that you use your mind. And we’ve looked and listened to your physical being, all the sensations that are going on your physical being. How sensitive you are. How much warmth, your circulation. The hesitancy when we move part of the body, the link with your eyes and your brain. The tone in that part of the body. And we've worked out what's going on, at that moment, to the best of our knowledge.
Only then do we decide on a tailor-made prescription for you, which can be a combination of many things. These may need to be in my clinic, or there may be a lot of things you can do at home as you don't really need us to be there for you, apart from just encouraging you along the way. It may also involve physical treatments, via just laying on hands, massage, that connection, dry needling, acupuncture, shockwave, manipulation, exercise advice. You name it, there's a myriad of physical hands-on treatments that we do.
We will write a prescription that's tailor-made just for you. It will be based on that moment in time, your immune system, your mind, your lifestyle and your available time. It will then progress to help your body get to the best you can be for your age, with whatever problem that you have. That is what tailor-made means. It means being listened to. And it means prescribing that medicine, be it in terms of a pharmaceutical drug, be it in terms of herbal medicine, be in terms in what we do, which is physically treating you and listening to you and looking at you holistically.
That's what we do.
If you are in pain right now and you feel confident we can help, then why not call. Erica, Jean and Charlotte will be happy to help.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
The Physical Assessment
In my three previous blogs on physiotherapy assessment
A Different Perspective On Your Physiotherapy Assessment
The Subjective Physiotherapy Assessment
The Subjective Physiotherapy Assessment - Part 2
I discussed concepts and steps which for most will not have been considered and most will have assumed that the physical assessment was the first step.
That is the mistake that so many make, missing out on the vital steps of creating the right environment to build connection and trust and gaining a deeper understanding of your important beliefs. Make that mistake and you are destined to gain so much less.
So the physical part of the assessment. What do we do? Well, in a private room we may ask you to take off some of your clothes, so you might want to be wearing clothes you're comfortable in and can take off quickly. If you're too shy to take off your clothes, just say it, it's not a problem.
Many of the assessments we make at my clinic are not common in the UK or anywhere else in the world. I am fortunate to have studied and qualified at the highest level in specific pain relief techniques and as a result I have learnt and ingrained advanced assessment techniques in myself and the rest of my team.
Then we'll be looking structurally at your skin. What does it look like? How healthy it is? What are the hairs like? Are there hairs missing? Does that mean the nerves are not working properly in that area? What's the temperature of the skin? Is it sweaty? Is it dry? How does the limb move? Does it move normally? If not, it will tell us is it’s likely to be arthritis in the joint that's blocking it. Or is it likely to be a tendon? Or a muscle or ligament? Or is it the nerves? Are they transmitting messages normally?
Or is it the brain? Has your brain created the pain felt in the body, possibly locked in from an emotional trauma many years earlier, even back to when you were a child? Chronic pain is created in many parts of the brain (evident in scans). Mindmapping physiotherapy techniques help to unwire the pain felt in the body.
So we're assessing the physical aspect. And that tells us so much about where we believe the problem is, or which systems are mostly causing the problem. Is it mostly the muscles? Is it mostly the nerves innovating the muscles? Is a blood flow problem? Is it something to do with what you are eating or if you don't move enough you are too weak. Or are you so stressed up, that you’re just pumping out inflammation into the area and you’re getting a more aggressive form of arthritis. And you don't need to. By looking at and at the same time feeling the response of your body, we learn a lot. If we hold a patient's hand that's sore, your eyes tend to move very differently than if you hold part of the body that isn't. Also there's a feeling about the hand, there's a hesitancy and there's a sort of a difference in the tone or strength.
There is so much in our senses, that we pick up on when we're assessing physically. Clearly this can only be done physically, face to face. Most of the above would be totally impossible to achieve by virtual means.
In my next blog Your Physiotherapy Prescription I’ll take you through how we develop a Physiotherapy treatment prescription, or plan, which takes you through the steps needed to achieve a successful outcome and let you get on with your life.
In the meantime, if you are in pain right now and you feel confident we can help, then why not call now. Erica, Jean and Charlotte will be happy to help.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
Ok, you are in pain, you have tried the obvious remedies, like pain killers and anti-inflammatories or a bit of exercise, but they didn’t fix the problem. You don’t want to be on drugs for too long, so you are thinking about getting to see a physiotherapist to assess you properly and find out what the problem really is and how best to fix it.
This presents you with a number of problems, such as where is the best physiotherapy clinic to go to and is it experienced with helping your type of problem. If you have friends or family who can provide help, based on their own experiences, then great. If not, the next best thing is to look at Google reviews and /or ask on social media. If you want some help on how to choose a clinic and what you need to ask, then click on this link How to Choose A Physiotherapy Clinic
You may have assumed that a physical assessment will be the first step.
That is the mistake that so many make, missing out the vital steps of creating the right environment to build connection and trust, and gaining a deeper understanding of your important beliefs. Make that mistake and you are destined to gain so much less.
Many of the assessment skills we use at my clinic are not common in the UK or anywhere else in the world. I am fortunate to have studied and qualified at the highest level in specific pain relief techniques and as a result, I have learnt and ingrained advanced assessment techniques in myself and the rest of my team.
Thus today, I want to approach this from a different angle, one you might not have thought of as being important, but trust me, it’s vital to a successful outcome. It’s the environment of the assessment room, and that means not only your room but the physiotherapists as well when the assessment is being done virtually.
You see, we all have an inherent ability to recognise if there is a true focus on the problem and that you are being listened to. If the environment is full of distractions or interruptions, then your physiotherapist’s thoughts will be disrupted and you will sense it. Your physiotherapist needs to be in the present moment, focussed and not allowing other thoughts to clutter up their head.
That’s my number one piece of advice.
Clearly, the environment is much better when you are face to face with the physiotherapist who is assessing you. There’s much less probability of distraction and that vital bond of trust is so much easier to build.
If your physiotherapist practices mindfulness techniques, they will induce a mental state capable of focussed attention on you. Your healing will commence as soon as you sense the caring intention.
I’m going to continue this explanation of how to achieve a successful assessment in more blogs. If you want me to keep with me on this journey, look out for my next instalment ‘The Subjective Physiotherapy Assessment’, which continues to look at this topic from a new perspective.
In the meantime, if you are in pain right now and you feel confident we can help, then why not call now. Erica, Jean and Charlotte will be happy to help.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
In my two previous blogs A Different Perspective On Your Physiotherapy Assessment and The Subjective Physiotherapy Assessment, I discussed the importance of getting that connection and really listening to get the patients story. Why are you here, what are your beliefs about treatment?
Now it’s time to go further, honing it down with specific questions about the problem.
Let’s use an example to help illustrate. Someone comes to me and they've had chronic pain in their foot for a very long time. I would be asking questions about the possibility of arthritis. Questions regarding the nervous system. Looking at the way that the body moves. Seeing if the pain is transmitting down from the spinal cord, because it could be a problem in the spine itself and not the foot at all. Having a look at the function of the foot, seeing if biomechanically the patient is walking in a strange way, and is that is making it worse?
How does it feel? How does the tissue feel? Is there any swelling? Are there problems with circulation? Is the sensation there? Are the nerves working properly? Is there an amplification of pain so that when I touch, the tissue is overly sensitive? What are the clues as to what's going on?
This is a very important start to this part of the assessment, which leads to the physical assessment.
To recap, the first part is establishing the connection and the story, the background, the beliefs, the values. The next part is to do with the Four Keys, to do with your immune system and your general health.
The next part is to hone it down into the particular problem today and how it's starting to manifest itself physically.
The final step is to go into the physical, which we can't do remotely by zoom. The physiotherapist has to get hands-on and assess physically, face to face.
In my next blog The Physical Assessment I will delve into the actual hands-on physical assessment. Many of you may have thought that this would be the first step in an assessment and that is the mistake that so many make, missing out on the vital steps of building connection and trust and gaining a deeper understanding of the all-important beliefs of the client. Make that mistake and you are destined to gain so much less.
In the meantime, if you are in pain right now and you feel confident we can help, then why not call now. Erica, Jean and Charlotte will be happy to help
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
I get asked a lot of questions about physiotherapy assessment. What do we do at my clinic? How do I assess? How do I teach assessing?
In my previous blog A Different Perspective On Your Physiotherapy Assessment, I mentioned that the first and most important thing is to have a safe, quiet environment that builds a connection and trust. If you don't feel that with your physiotherapist, you're not going to want to proceed to any kind of medicine or treatment and your outcome won't be as successful. There won't be that connection.
To recap, the most important thing for the patient is that the physiotherapist has created a sacred space, a quiet office, where the phones are switched off, the computer is not a distraction, and you eyeball each other to get that connection. And then your physiotherapist listens to your story. And how you describe what's going on with you. And then, in that moment of connection, your physiotherapist can get glimpses of the real authentic self behind the story, who you really are.
Once your physiotherapist glimpses the story of the problem, he or she can start to elicit some background which is past medical history. So we'll ask questions like the health of your family to see if there are relevant genetic links. We may also explore your beliefs and values and more about your family so we'll know how difficult it is for you to attend and for you to have the necessary treatment. We may touch on your past experiences of treatment because if you've been scared or let down previously, you're going to have very different expectations. We need to address that head-on.
And then, of course, my favourite four keys questions (see my first book ‘The Four Keys To Health’ available on Amazon), which looks into your mindset, lifestyle, fitness and what you eat. All these help us assess how well your immune system is working, and your general health, which helps refine our treatment prescription.
That, in a nutshell, is the first part of the physiotherapy assessment.
In my next blog ‘The Subjective Physiotherapy Assessment – Part 2’ I will continue on this journey of helping you understand how to really get the most out of this process.
In the meantime, if you are in pain right now and you feel confident we can help, then why not call now. Erica, Jean and Charlotte will be happy to help.
Call 01889 881488 Now
p.s. Don’t try to book online at this time as that is only suitable for existing clients already being treated for an existing problem.
