One of the first questions any patient asks when obtaining an injury is ‘how long until it gets better’... If only an answer were simple.
Unfortunately, when it comes to the shoulder joint, the answer isn’t straightforward at all because your shoulder is one of the most complicated joints in your body.
To achieve the wide range of movement that the shoulder provides, it requires a combination of muscles from body to shoulder blade (scapula), body to arm bone (humerus) and shoulder blade to arm bone. Due to this complexity, it is one of the most susceptible joints in the body to injury.
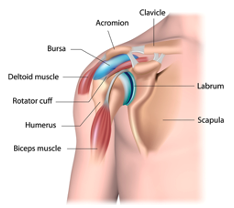
The shoulder is made up of three bones, the upper arm bone (humerus), the shoulder blade (scapula) and the collarbone (clavicle). There are joints between the clavicle and scapula and between the scapula and humerus.
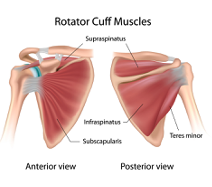
The stability of the shoulder is predominantly controlled by four muscles, commonly known as the rotator cuff. They are tasked with keeping the joint properly centred and located.
 These are
These are
- Supraspinatus
- Infraspinatus
- Subscapularis
- Teres Minor
Common Shoulder Problems
The most common shoulder injuries are:
- Rotator cuff tears/tendonitis
- Impingement
- Instability
- Frozen Shoulder
- Bursitis
- Osteoarthritis
Rotator Cuff Tears
The rotator cuff muscles and tendons are an important part of the shoulder and are tasked with keeping the bones of the joint together across its wide range of motion. Rotator cuff tears account for more than 50% of shoulder injuries and are most common in people who repeatedly perform overhead motions. Thus athletes involved in sports such as swimming, racquet sports and weight lifting, which all require repetitive overhead movement, are particularly prone to injury.
Typical symptoms of a rotator cuff tear will be pain at night disturbing your sleep, and probably some lessening of pain during the day, although any overhead movement or even reaching behind your back is likely to be painful. You will also probably experience weakness in the affected arm. If left untreated, the pain will most likely increase over time.
Keen athletes may be tempted to continue in their favourite sport, in the hope that the pain will recede, but this will most likely aggravate the situation and, over time, may make the condition worse. If you suspect a rotator cuff tear, it is strongly advised to seek help from a qualified physiotherapist or sports therapist as soon as possible, as some conditions, such as a full-thickness supraspinatus tear, can become irreversible if left too long.
Impingement
Rotator cuff tendons can become trapped between a bony projection of the shoulder blade called the acromion and the top of the humerus (arm bone). Particularly prone is the supraspinatus tendon, this muscle is responsible for moving the top of the arm sideways from the body for about the first 15 degrees of arm movement.
Impingement problems can be caused by a number of factors, including:
- Loss of scapula – humeral rhythm
- Nerve interference or injury from the neck to the shoulder, causing abnormal movement of the shoulder
- Poor posture
- Tears and inflammation of tendons
Instability
Recent dislocation, sudden injury or overuse can each cause shoulder instability. The head of the upper arm bone can glide out of the shoulder socket (glenoid). This can occur when the capsule and ligaments that have the role of stabilising the shoulder in the socket have not healed properly and remain stretched making them too loose to keep the shoulder stabilised. This can result in repeated dislocations.
It is, therefore important to seek treatment. Rehabilitation and soft tissue work can be provided by qualified physiotherapists or sports therapists to help strengthen the muscles and ligaments and help to gain stability around the shoulder joint once more. It is advisable to seek help sooner rather than later.
Frozen Shoulder
This condition, medically described as adhesive capsulitis, can literally develop overnight. The capsule of the joint becomes inflamed and stiff, resulting in restricted movement. Eventually, the shoulder ‘freezes’ and becomes immobile for a few months to a year.
However, a frozen shoulder does typically progress in three main stages:
- Freezing stage- any movement of your shoulder causes pain, and your shoulder's range of motion starts to become limited.
- Frozen stage- pain may begin to diminish during this stage. However, your shoulder becomes stiffer and moving it becomes more difficult.
- Thawing stage- The range of motion in your shoulder begins to improve.
Bursitis
A bursa is a fluid-filled sac that act as a cushion to stop friction between the muscles and bones as they glide over on another. You have several in your shoulder, one being one of the largest in the body which is located towards the top of the arm.
After an excessive repetitive motion of the shoulder, the bursas can inflame and swell. The pain is normally a gradual onset located on the outside of the shoulder which can spread down the arm. It can become more aggravated when lying on the shoulder or if you’re using your shoulder anywhere from 60-90 degrees up and outwards.
When treating Bursitis, the aim is to control the inflammation. If you don’t seek help, often the pain will become worse and become impinged.
Osteoarthritis
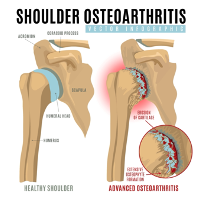 This is when the normally smooth cartilage that covers the ball and socket joint diminishes after constant friction leaving bone to grind against bone. It develops slowly and the pain worsens over time, normally after chronic wear and tear or work injuries. Symptoms may include swelling, pain, and stiffness.
This is when the normally smooth cartilage that covers the ball and socket joint diminishes after constant friction leaving bone to grind against bone. It develops slowly and the pain worsens over time, normally after chronic wear and tear or work injuries. Symptoms may include swelling, pain, and stiffness.
Osteoarthritis is a chronic problem which cannot be resolved, but the symptoms of the condition are amenable to pain-reducing treatment.
Every shoulder injury will present differently, and everyone’s perception of improvement will be different too. For example, one patient may be over the moon for gaining an extra 10 degrees in pain-free shoulder motion. Whereas the next will be happy only when gaining their full range of motion back.
Many biological, psychological, and social factors are involved during the recovery process after a shoulder injury.
If you are suffering from shoulder pain, we can help
Call 01889 881488 Now
Jean, Erica & Charlotte will be happy to help
The knee is the body’s largest joint and made up of four bones; the shin bone (tibia), the thigh bone (femur), a smaller bone on the outside of the leg (fibula) that attaches to the shin bone and helps support body weight, and the knee cap (patella). The knee joint is called a hinge joint, as it can bend, straighten and twist.
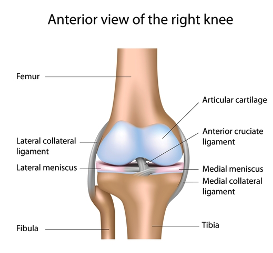
Each of the ends of the bones in the knee are covered in cartilage to protect the bones and let the joint move smoothly. Between the bones in the knee, there are 2 wedge-shaped pieces of cartilage, called meniscii. These are the shock absorbers and help cushion the joint from impact.
The knee joint is held together by ligaments which make the joint stable. There are four main ligaments in the knee. There are the collateral ligaments which run down the sides of the knee, which help to limit sideways movement of the joint and support against unusual movement. Then there are the cruciate ligaments, which are inside the knee and cross each other, to control back and forth movement in the joint.
Another factor in knee stability is muscles which also provide power and are the reason the joints can move. The knee is surrounded by strong muscles. The quadriceps are the front thigh muscles and they work to straighten the knee. If they are weak then this can lead to instability of the knee and kneecap. The hamstrings are the muscles on the back of the leg and their job is to bend the knee.
Which are inside the knee and cross each other, to control back-and-forth movement in the joint.
Another factor in knee stability is muscles which also provide power and are the reason the joints can move. The knee is surrounded by strong muscles. The quadriceps are the front thigh muscles and they work to straighten the knee. If they are weak then this can lead to instability of the knee and kneecap. The hamstrings are the muscles on the back of the leg and their job is to bend the knee.
Common knee injuries/conditions:
Knee ligament injuries – Normally from an accident, whether a slip, trip or fall. As mentioned above there are several different ligaments that support the knee. If you think you may have injured one, it is important that you see a Physiotherapist/Sports Therapist who can examine your knee to diagnose which ligament is damaged and how badly.
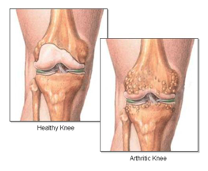 Osteoarthritis - wear and tear of the cartilage in the knee is called Osteoarthritis and is a common cause of pain. It may be aggravated by biomechanics, previous injury, overuse or the simple effect of years of living. Osteoarthritis symptoms can be relieved with orthotics, exercise and pain-relieving treatments.
Osteoarthritis - wear and tear of the cartilage in the knee is called Osteoarthritis and is a common cause of pain. It may be aggravated by biomechanics, previous injury, overuse or the simple effect of years of living. Osteoarthritis symptoms can be relieved with orthotics, exercise and pain-relieving treatments.
Cartilage injuries – often caused by sudden twisting, the cartilage between the knee can get damaged. If this is the case the knee needs strengthening and there may be a chance that surgery is required. It is crucial that you have a proper assessment to determine the best course of action.
The Impact of Leverage
When we can’t undo a tight nut, we reach for a longer spanner to give us more leverage. It’s a concept we all understand.
This same leverage principle applies to our knees as well because for most of the time the centre of our weight is not directly over our knees. Try looking sideways in a mirror and bend your knees and you will see that your knees are in front of the trunk of your body. Hence your body weight is applying leverage on your knees. As you bend your knees further, your knees get further in front and the leverage increases, just like using a longer spanner.
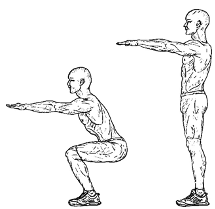
The implications of this leverage are that in normal walking your knees have to support 4 times your weight. If you crouch down it can go as 9 times your weight. No wonder then that if we carry excess weight, our knees will take the brunt of that, which means that knee problems are likely to be more likely with excess weight.
The good news is that most of us have the capability to do something about our weight. A simple change in diet and a bit more exercise is all it usually takes. And, of course, the motivation to do this.
Most common knee injuries in sports
The knees are frequently injured due to the stress of frequent starts, stops, twists and turns applied to the joint during exercise.
- The most common injury in the knee is knee ligament injuries. This normally occurs from an accident, whether a slip, trip or fall. The ligaments’ main role is to stabilise the knee so the knee might experience a sudden twisting motion, a rapid change in direction, or an incorrect landing from a jump. Sometimes you can hear a pop, or a snap followed by swelling and a loss of range of motion. It is important to see a physiotherapist/ sports therapist who can examine your knee to diagnose which ligament is damaged and how badly, so we can treat it sooner rather than later.
- Another common injury is to the meniscus (shock absorbers) of the knee. This can happen from general aging where the meniscus has become weak and tears after an awkward turn during normal day to day activities. Or it can happen during sports where the knee twists and pivots. You will normally feel pain, stiffness, locking and a decreased range of motion.
- Meniscus damage can take time to heal and can get worse over time if it isn’t treated properly by a physiotherapist/ sports therapist. It is crucial to have a proper assessment to determine the best course of action.
Overuse injuries are also common, including ‘runners’ knee’ or osteoarthritis.
- Runner’s knee is common in runners and cyclists. You often have dull pain around the front of the knee and can feel like a rubbing, grinding, or clicking sound in the knee cap. Your physiotherapist/sports therapist can help treat runners’ knee through a combination of massage and acupuncture. This will help relieve some of the pain and break that vicious cycle.
Looking after yourself and keeping healthy will most likely keep knees healthy too. Getting help sooner rather than later will also help massively with recovery time and getting you back to your day-to-day pain free activities.
If you are suffering with knee problems, you really need to see a physiotherapist/sports therapist sooner rather than later to correctly diagnose and then provide the best treatment possible.
Call 01889 881488 Now
Erica, Jean and Charlotte will be happy to help
The elbow joint is a synovial hinge joint in the arm and consists of three main bones: The humerus of the upper arm, the radius and ulna of the forearm. The elbow joint enables us to bend and straighten our arm.
Tennis Elbow
This is a condition that causes pain on the outside of your elbow. It is mostly caused by overusing your forearm from repetitive or strenuous motions. If these motions are a normal part of your daily routine, then resolving your tennis elbow pain can involve quite a lot of time and treatment. In the interim, you may only get bouts of temporary relief. Permanent relief will probably necessitate a change in your daily routine and a fair degree of patience. Needless to say, tennis elbow problems should always be referred to qualified therapists with access to suitable technology, such as shockwave.
A simple but effective exercise involves doing light twists of the arm and bicep curls using a lightweight. The goal is to strengthen the tendons and the muscles in you arm. You can also stretch out the forearm by placing your fingers on a hard surface and pressing downwards, stretching out both the hands, the wrists, and the forearms.
Self-massage can also be helpful and can be found on YouTube. We also offer sports massage therapies in the clinic, ask for details
Golfers Elbow
Now the difference between tennis elbow and golfers’ elbow is that tennis elbow is inflammation of the tendon where it joins to the bone in the outer elbow and golfers elbow is inflammation of the tendon where it joins to a bone in the inner elbow.
Both injuries are overuse injuries that are caused by activities that require repetitive motion of the arm and wrist. The problems of resolving pain from golfers elbow are the same as for tennis elbow, covered above.
Occasionally, for both golfers and tennis elbow you may wear an elbow brace. The purpose of the brace is to redirect the pressure over your muscles so that the injured area doesn’t take full force.
Bursitis
 There are many bursae located throughout the body that act as cushions between bones and soft tissues, such as skin. They contain a small amount of lubricating fluid that allows the soft tissues to move freely over the underlying bone.
There are many bursae located throughout the body that act as cushions between bones and soft tissues, such as skin. They contain a small amount of lubricating fluid that allows the soft tissues to move freely over the underlying bone.
Sometimes the bursa may become irritated or inflamed, more fluid will accumulate in the bursa and a bursitis will develop. It becomes swollen, painful and worsens with direct pressure on to the elbow. The swelling can sometimes grow large enough to effect range of motion. It can also become red and warm to touch.
At Nicky Snazell’s clinic, you can receive two treatments for bursitis that will help alleviate acute and chronic pain. Deep oscillation and pulsed shortwave.
- Deep oscillation provides an electrostatic current that helps to increase blood flow, circulation and helps to enhance treatment outcomes as it proves symptomatic relief.
- Pulsed shortwave acts as a type of microwave that provides a high frequency electromatic energy into the body to help reduce pain and swelling. It works particularly well for bursitis.
A soft pad can ease discomfort.
Ulna nerve irritation
This occurs when the nerve in the arm becomes compressed or irritated. The ulna nerve is one of the three main nerves in the arm. It travels from your neck down into your hand and can be constricted in several places along the way.
The most common place for compression of the nerve is behind the inside part of the elbow. Ulnar nerve compression at the elbow is called ‘cubital tunnel syndrome. It can cause numbness and tingling sensations in the hand and fingers.
However, you should seek help from a therapist as there are a number of reasons you may be getting these symptoms. More often than not, the pins and needles sensation you may feel, in your hand, for example, can be coming from a different area of the body completely. It may just be referred pain you are experiencing.
Top tips to reduce the likelihood of elbow injury
- Seek early advice from a physiotherapist or sports therapist.
- Protect your joints during activity, especially during winter activities. Wear elbow pads and wrist guards
- Don’t throw through elbow pain.
- Maintain a good posture- this prevents elbow injuries from compensatory overuse.
- Consider a workstation set up, as elbow pain can develop with prolonged daily computer use with poor posture.
If you are in pain, we can help
Call 01889 881488 Now
Jean, Erica & Charlotte will be happy to help
How can I relieve neck pain? The first thing to understand is how this happened, neck pain can be caused by other conditions such as muscle weakness in the shoulders, perhaps lifestyles such as workplace seating or even sports. Take a moment to consider what could be causing yours. While doing this, think about the type of pain you have. Is it a strain or a trapped nerve?
What does a trapped nerve in neck feel like?

A trapped never typically feels more painful in certain positions, and the pain again can be shooting, described as electric or pulsing. A trapped nerve can throb and jolt when you are moving. A strain usually feels more like a burn or a tear; these sensations can be confusing, so please do not worry if you struggle to distinguish between the two - Our team can help you understand this better and decide the best ways to help you.
How long does neck strain take to heal?
A strain can take between 24-hours and a week to recover. If you are concerned Nicky Snazell can help you with pain relief, it is still worth considering what caused this. The underlying source is always the best way to provide you with long-term pain relief, and maintenance can reduce reoccurrence.
What is the fastest way to fix a stiff neck?
If you are not ready to consider treatment, we recommend gentle stretches and a gentle massage in-between cooling and warming treatments like an ice-pack and a hot water bottle/wheat/rice bag. Be careful when doing this yourself. If you are unsure how to manage this effectively, contact us.
Which massage is best for neck pain?
This depends on how you got the neck pain; if it was doing sports, then as you might expect, sports massage could be the proper treatment. Typically, massage is the right treatment for neck pain; manipulating the soft tissue can relax the problem and promote blood flow and healing.
Where can you go for help with neck pain?
Nicky Snazell pain relief clinic in Stafford can help with neck pain. Please view this page for more information on neck pain, or contact us. Our experienced team of physiotherapists will help you navigate your pain and provide the most effective advice to help you long term.
Availability Of Treatment Has Never Been More Important
With the daily media bombardment about COVID, it is no wonder that fear is generally growing. Fear of the social impact of another lockdown, fear of the uncertainty of our livelihoods and even fear of our very existence. Staffordshire has announced that it will go to Tier 2 at midnight on Friday and this will inevitably raise the fear factor higher.
Mental health has taken a back step with this pandemic and never before in my working life has there been so much anxiety, loneliness and grief hidden away in society.
Your pain, whether physical, mental or both, isn’t going to disappear and many of you are going to need a lot of help in the coming months. Increasingly, we are being asked to help guide people through these difficult times both mentally and spiritually, the latter problems only serving to multiply the actual physical pain.
We Are Staying Open
We know that stress lowers our immunity and raises our sensitivity to pain. Gold standard trials have also proven a relationship between lifestyle stressors and white cell count. What this means is that stress, if left untreated, will slow down your ability to heal, plus worsen your response to pain, inflammation and disease. Yet psychosocial pain is, I believe, wrongly still an afterthought in western medicine, even though more often than not, it holds the key to hidden trauma and deep emotional stress.
At this clinic, we have long recognised the importance of looking at the whole person, rather than just the location of pain. That’s why, even though I am highly qualified in western medical techniques, I have written 5 books on a more holistic approach. In my first book, The 4 Keys To Health, I introduced a simple traffic light scoring system which encompassed the psychosocial factors that affect our health and which can cause so much of our pain.
Our goal is thus to help people in all aspects of their health and never before in my lifetime has there been such an urgent need for this approach. Beyond treating your pain, we wish to get you to as close optimum health as possible to help protect your immune system.
That’s why at the clinic we love to build a relationship with our clients to prescribe a tailor-made treatment plan, working out the best way to help with the mind set and adding in massage, and technology such as laser, shockwave, deep oscillation, acupuncture and IMS dry needling.
Keeping Abreast Of Research
We are constantly monitoring recent research to find new techniques to help. As an example, a recent Harvard trial successfully used electroacupuncture to improve survivability in COVID infected mice. This is highly relevant research, as in some cases it has been shown that it is the human bodies over response to COVID infection which has caused excessive inflammation [cytokine storm], leading in some cases to death. The research findings are significant. Electroacupuncture treatment before the cytokine storm increased survivability by a factor of four, from 20% to 80%. When applied after the cytokine storm, survivability increased by three-fold, from 20% to 60%. Both are huge benefits and it emphasises the benefit of preventative treatment.
As a result of our integrative approach to treatment, combining orthodox western medicine with alternative, we routinely carry out electroacupuncture here.
For those of you who need our help, we are open and will continue to be open unless forced to close by government ruling.
None of us know how long this pandemic is going to last, but the expectation is that it’s going to be a long time. If the availability of treatment is shut off there is going to be a drastic rise in pain and suffering. We have already seen this in the lockdown with patients begging us to see them. That’s why I believe it is so important that we stay open in the coming months.
Our patients are so grateful that we are here now to help them with their pain, pain they suffered for months without any help during lockdown. They have bombarded us with thanks. We will continue to stay open and help you unless and until the government dictates otherwise. Sadly, the chances are there will be few, if any, alternatives for you.
Control Your Stress Now And Improve Your Resistance To Disease
While the government is correct to react to rises in cases, we each need to keep in perspective what the tier trigger points represent, so that we can keep better control of our stress. Tier 2 is triggered at 100 per 100,000 population. Put another way, on average you would need to get close to 1000 people before you are likely to be near a COVID positive risk. How likely, if you are careful, are you to interface closely with 1000 people, especially in these troubled times? Maintain social distancing and always wear a mask to reduce your chances of infection further.
What does this tell us? Mix only with people you are reasonably sure act sensibly and act sensibly yourself. Nothing is guaranteed in life, but by acting sensibly and taking all possible precautions, you can use your own positive response to improve your health.
What We are Doing About COVID-19 At Nicky Snazell Clinic
COVID-19 has had a dramatic affect on all our lives and not surprisingly at Nicky Snazell Clinic as well. Our foremost concern is the safety of patients and staff and we strive to stay fully up to date with the almost daily changes and wherever possible keep ahead of the curve. More on that later.
Screening
Even if you are an existing patient, but definitely if you are a new patient, we will take you through a screening process to make sure it is safe and justified for you to come in for treatment. There will be quite a few questions, and we ask you to bear with us on this as it’s all in our best interests. For sure, the questions asked will constantly change in line with latest guidelines. Where the risk is deemed higher, then a more detailed assessment will be needed with a physiotherapist, before treatment can be authorised.
Please note that in cases where you may need to be accompanied, then that person also has to pass screening to be allowed on site.
Changes At The Clinic
All of our 13,000 plus patients will know that our aim has always been to create a welcoming, peaceful and relaxing environment from the moment you walk in the door. Well that of course, to an extent, went out the door when we adjusted rapidly to the pandemic. Our waiting room has been effectively closed and patients are now asked to wait in their cars until their allotted start time. At that point they should come in alone with a face mask on, use the readily available hand sanitiser and their therapist, wearing full PPE, will take them to the treatment room.
At the end of the appointment the therapist will, if necessary, book a follow-on appointment and we then ask that you go to reception, where we have installed protective screens, to pay in advance for the next appointment. To speed this process, we now only take payment by card and by touch whenever possible. Where a payment requires a pin, the terminal is sanitised after use.
We then ask that you leave the clinic immediately as we want to minimise time that patients are in the clinic. Please don’t think we are being rude if we don’t chat as we used to. We are minimising your time on site. We have also staggered the start times between therapists, to avoid multiple patients being on site outside of a treatment room at the same time.
Cleaning
All rooms are sanitised between treatments and thus treatment times will be slightly shorter. In addition, we use a spray which lasts up to 5 hours on surfaces and this is used on all common touch points every 3 hours. Thus, for example, when you open the door to come in, you can be sure that the handle and surrounding woodwork will have been sprayed and is as safe as is practical.
We understand of course that some patients will need to use the toilet and we request that if needed, you first advise us so that we can sanitise after each use. Note, however, that the toilet is also thoroughly sanitised every 3 hours with our 5 hour effective spray. Please try to avoid the need to use our facilities wherever possible.
Your Part
We require that you use a face mask which covers your mouth and nose at all times while inside the clinic. All of the available scientific information supports the need to wear masks inside a building. It is important for each of us to realise that wearing a mask helps protect those around us from us. By not wearing a mask properly, this would be putting our staff at additional risk and this is not acceptable.
Patients at times have found difficulty in wearing a mask, but we politely request that you must do so for the short time on site. Bear in mind that our staff are in full PPE all day to protect you.
Patients who do not comply with this request may be refused further treatment.
We also need your help in running to time. It is vital that you have vacated the treatment room on time, leaving sufficient time for the room to be sanitised. Any overrun will mean that patients will be held in the waiting room and this is not acceptable.
Payment In Advance
We have changed our payment procedure, as we now ask for payment in full at time of booking and in 99.9% of cases this has been fully understood and accepted. On one or two occasions, however, patients have misunderstood our reasoning for this. We have made this change by necessity, as many patients leave the building immediately after their treatment and it would be totally unworkable for us to have to continuously call patients to take payment. We had to come up with a single system for all, so this change is not a reflection on any one patient.
Staying Ahead Of The Curve
Part of our role is to stay up to speed with the ongoing changes caused by our government updates, but in addition, we, and in fact all of us, can choose to operate more safely if we wish. An example would be that last night Scotland announced that most COVID-19 infections were caused by meeting people from outside our household within our homes and thus banned this. In England a more relaxed position has been taken. It is, however, up to us to decide which position is more in our best interest. If we at the clinic feel it worthwhile to use more strict guidelines to help protect all, then we reserve the right to do so.
Having lived in the USA twice, I personally check in on their news channels and in particular I look for information from Dr Anthony Fauci, who is the USA’s leading disease expert, having been advisor to the last six Presidents. He talks more openly and simply than we tend to get in the UK. He is also completely apolitical and is only interested in scientific proof. There is also a wealth of real world, scientifically based information put out by Dr Sanjay Gupta.
Yesterday Dr Gupta interviewed Dr Fauci and for those who want a better insight and understanding of where we are right now, then I recommend you watch the interview on YouTube.
For those who don’t have time to watch this, here are some snippets:
- Dr Fauci is optimistic that a vaccine may be ready for approval by November or December, based on the limited results available in the small-scale phase one and two trials. But, and this is a big but, the all important large scale phase 3 trials are double blind, placebo controlled trials and so even he has no idea what the current results are. In fact, nobody does, except one or two statisticians who see unblinded results. In simple terms, a double blind trial means that only the statisticians know who is getting the placebo and who is getting the vaccine being tested, not even the manufacturers, as the trial is conducted by an independent group. This is the gold standard for scientific testing and is not something that can be politically manipulated.
- The best advice is that we must all wear face masks if social distancing can’t be maintained.
- What we didn’t know a few months ago was that 40% to 45% of COVID positive people were asymptomatic, nor were we aware that a substantial proportion of the infections were coming from those who were without symptoms. That makes it overwhelmingly important to wear a mask.
- There is a suggestion that some of the virus droplets in the air may be light enough to hang around and circulate, thus acting as an aerosol. The facts are we don’t know yet, but in many respects, it doesn’t matter. It just emphasises the advice given: wear a mask, keep your distance, avoid crowds, wash hands regularly, ventilate rooms.
- Yes, the elderly are more at risk, but people with underlying conditions, at any age, are at risk.
The overwhelming issue is that we all need to get on with our lives while we minimise our risk during this pandemic. We believe we are taking every possible step to minimise that risk and that we have created a far safer environment than most.
Take care, be safe, think of others
Spinal Disk Bulge Physiotherapy For A Spinal Disc Rupture
Can a disc slip? The simple answer is no. It’s a layman’s term that is unfortunately very misleading to the general public.“My disc has slipped out, can you put it back in” is not an uncommon conversation opener on the telephone. Of course, it’s quite difficult then to get the caller to understand that this can’t actually happen, which is why Spinal Disk Bulge Physiotherapy is key to recovery.
Let’s look at the spine’s anatomy and in particular the role of the disc.
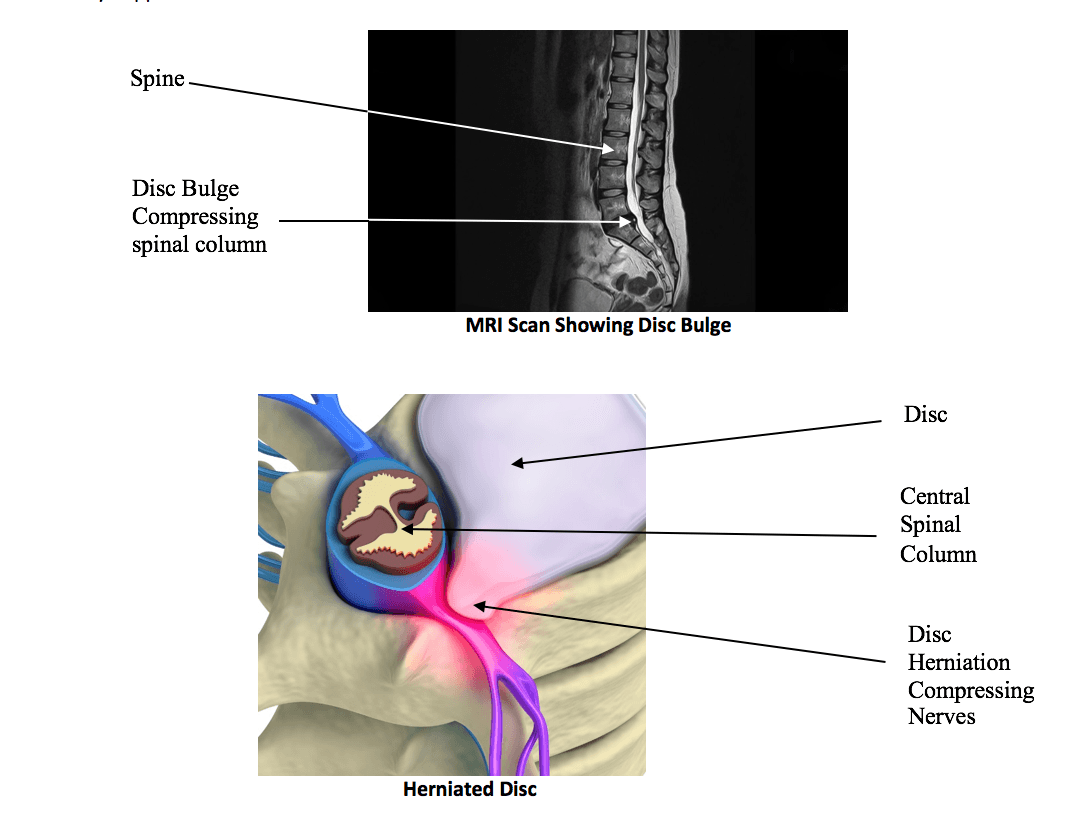
The spine is made up of 7 cervical (neck) bones called vertebrae, 12 thoracics (middle) vertebrae and 5 lumbar (lower) vertebrae. The top 2 vertebrae in the neck are a little bit different, so putting those to one side, between each pair of the remaining vertebrae there is a disc, the purpose of which is to provide shock absorption and allow movement. The disc itself is attached strongly to the vertebrae and cannot slip out.
A disc is made up of a tough fibrous structure on the outside, layered in exactly the same way we make cross-ply tyres. On the inside, there is a soft, crab paste-like moist material. As we age this tends to dry out. There are also endplates in contact with the vertebrae. The spinal disc is 70% to 90% water, so making sure you are well hydrated is very important to disc health.
There are two major types of damage to these discs. The first is when the disc is overloaded sufficiently to cause a protrusion, or bulge in the outer wall, as in the diagram above. This is similar to what you see on the side of a car tyre when it has hit a curb. Sometimes this is referred to as a slipped disc. It’s not possible to just push the bulge back in, but specific exercises can help to relocate this and over time the disc may heal itself.
The second and more serious damage is when the overload has been sufficient to rupture the outer fibrous structure and force the inner material to squeeze out. This is called a herniated or ruptured disc.
What Are The Implications Of A Disc Bulge Or Herniated Disc?
A disc bulge will cause pain if it is central and compresses the central spinal column, or if it bulges to one side into the exiting nerves. In either case, if the compression is significant enough, it will cause pain and/or numbness and weakness and possibly loss of control in the limbs.
If the disc bulge is central it could cause problems down both sides of the body. If the bulge is on one side, it will only cause problems on that side.
If the disc has been ruptured or herniated, the same problems with compression of the central spinal column and exiting nerves can occur. In addition, if chemicals from the inside of the disc come into contact with the nerves, it can cause severe pain even without any compression of the nerves. In such cases, a course of anti-inflammatories will most likely be prescribed.
Can Spinal Disk Bulge Physiotherapy Treat A Disc Bulge or Herniated Disc?
In many cases, a bulging disc and a herniated disc will over time heal themselves. The time required may depend on the severity of the problem and may take from weeks to months to resolve. Physiotherapy treatment can help reduce the pain much more quickly. The key is to get an accurate diagnosis through a physiotherapy assessment, possibly needing an X-ray or MRI. Treatment can include specific exercises to help reduce the disk bulge, Gunn IMS dry needling, electroacupuncture, laser, shockwave, core stability rehab and postural rehab. In severe cases, surgery may be needed.
If you have suffered a recent back injury or had a long-term problem then it’s advisable to get your condition assessed and treated. We have extensive skills in treating spinal pain and clients travel from all over the UK and abroad to seek our help.
Call 01889 881488 now.
